The Neurology Behind A Hyperactive Mind: ADHD
- Raihanna Osayra Rafinal
- Nov 24, 2025
- 5 min read
What is ADHD?
Nowadays, the terms ‘ADHD’, ‘OCD’, and autism get thrown around in everyday conversation. Sometimes, we might forget that these are actual detrimental conditions that affect people’s daily lives, and for some, severely.
ADHD, short for Attention-Deficit Hyperactivity Disorder, is one of the most common disorders in children, according to Boston Children’s Hospital (2024). The cause of ADHD is a genetic change that causes neurodivergence: differences in how the brain normally develops. This genetic change is highly heritable and may affect other cognitive functions such as working memory and attention (Ribasés et al., 2023).
Accordingly, the symptoms of ADHD include: hyperactivity and impulsivity, as the name would suggest. Hyperactivity includes being unable to stay still, while impulsivity may lead to an inability to think things rationally before following through with an action (Attention-Deficit/Hyperactivity Disorder: MedlinePlus Genetics, 2019). This inability to focus on tasks frequently becomes so severe that it interferes with school, work, and relationships, as they have difficulty in time management and following through with deadlines. This could lead teachers or co-workers to chalk it up as ‘lazy’, yet it is actually a significant challenge faced by those with ADHD every day, one with, in contrast, too many thoughts behind every action. To even wake up and eat takes a lot of thinking, time, and effort, which could also be due to their tendency to avoid tasks requiring large amounts of attention.
The trend of using actual disorders, such as ADHD, as hyperbole to explain neurotypical behaviour, such as lack of focus, creates a stigma where the struggles of ADHD are devalued and its complexities are misunderstood. Some people even go as far as to say those who claim to have ADHD are only fishing for attention. So here, we’ll pull back the curtain and reveal the scientific gears behind an ADHD brain, appreciating their unique flow of thoughts instead of dismissing them.
The Science Behind It!
Since ADHD is a neurological disorder, most of the causes of ADHD are due to the difference in neurotransmitters and areas of the brain, compared to a non-ADHD brain. Neurotransmitters are chemical messengers that cause an impulse to be transmitted between neurons in the brain. These impulses regulate neural signaling responsible for attention, behavior, and decision-making. An example of a neurotransmitter is norepinephrine, which accounts for attention and arousal, regulating impulsivity by influencing response control. Naturally, ADHD brains have lower levels of norepinephrine than non-ADHD brains, explaining the lack of impulse control those with ADHD experience. Norepinephrine is synthesized from another neurotransmitter, dopamine, which plays a critical role in behavioral regulation, motivation and reward processing. Following this, low levels of both norepinephrine and dopamine are linked to ADHD, explaining difficulty in maintaining motivation to finish tasks, causing those with ADHD to jump between several different hobbies for short periods of time. This also explains why the ADHD brain favours immediate awards over long-term future ones (ADDA Editorial Team, 2022).
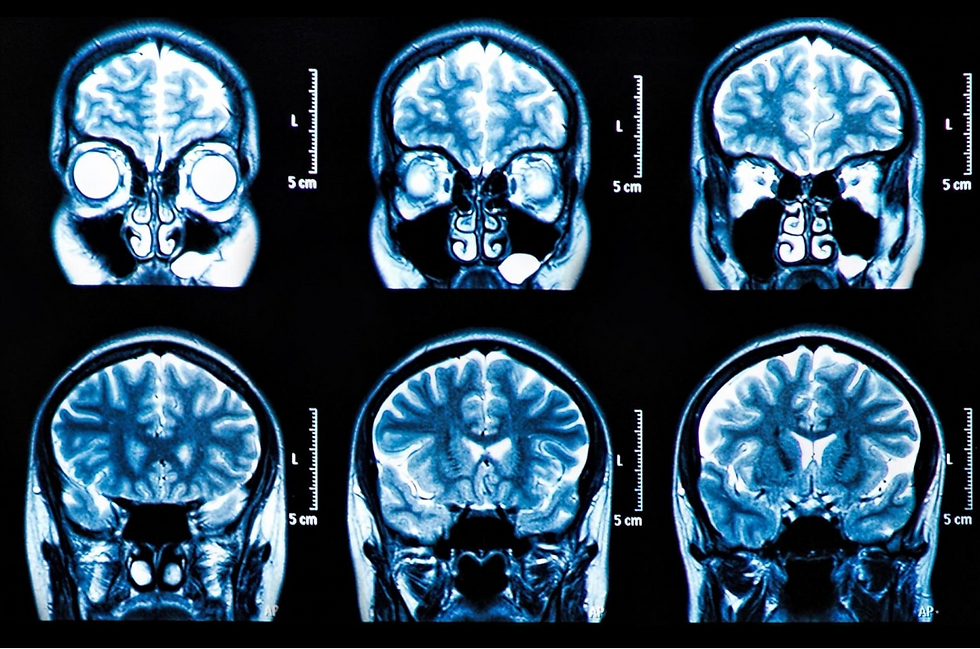
Aside from chemicals in the brain, the structure of the ADHD brain also differs! The frontal lobe is largely affected by ADHD, slowing its development, disrupting neural connections and activity (ADDA Editorial Team, 2022). The frontal lobe includes the prefrontal cortex (PFC) and is heavily involved in dopamine signaling (Villines, 2023).
Bayard et al. (2018), which aimed to test whether brain structure was specifically associated with ADHD in adolescents, found decreased gray matter volume and surface area in the prefrontal cortex (PFC) linked to ADHD. Gray matter is where most of the brain’s neuronal bodies are, processing information to integrate and coordinate sensory and motor senses following brain impulses. Gray matter in the PFC plays a large role in controlling attention, decision-making, and control over impulsive behaviour. So, a decrease in gray matter in the PFC can lead to less control in many aspects of behavior, such as emotional regulation, attention, cognitive control, and executive function.
ADHD Treatment?
With such chemical and structural changes in the brain, is there a way to cure–or at the very least–temporarily reduce the effects of ADHD? The answer is: yes! Of course, these treatments aren’t permanent, and won't be the solution to all of the problems ADHD brains face, but they could still prove beneficial in certain situations where ADHD becomes a large nuisance.
In terms of medication, they are commonly either stimulants or nonstimulants. Stimulants–as the name suggests–directly stimulates the nervous system and its activity. They are more commonly used as they are usually more effective to treat ADHD symptoms (Rodden, 2019). They increase dopamine and norepinephrine levels in the brain, accounting for the usual lack of such neurotransmitters, for example, Adderall (Lockett, 2022). Nonstimulants, as opposed to stimulants, do not directly stimulate the nervous system, rather they use other pathways to manipulate neurotransmitter levels. Nonstimulants also improve symptoms of ADHD by changing other neurotransmitter levels, such as decreasing selective norepinephrine reuptake inhibitors (SNRIs) that block the reabsorption of norepinephrine into neurons (Miller, 2023). Nonstimulants may be a useful alternative for those who experience severe side effects when using stimulants.
Conclusion
So, ADHD does indeed have a neurological explanation behind it, proving how their brain is wired differently from a non-ADHD brain. Due to their disorder, they may come off as irresponsible and reckless, but in reality, their brain is constantly fighting their will to complete tasks on time like everyone else. To promote an understanding of the ADHD brain, more awareness to reduce the stigma behind those with ADHD should be spread, starting with you! If you happen to know someone with ADHD, try to understand their thought process, and maybe you can both benefit from understanding how differently your brains work.
References:
ADDA Editorial Team. (2022, December 20). Inside the ADHD brain: Structure, function, and chemistry. ADDA - Attention Deficit Disorder Association. https://add.org/adhd-brain/
Attention-deficit/hyperactivity disorder: MedlinePlus Genetics. (2019, July 1). Medlineplus.gov. https://medlineplus.gov/genetics/condition/attention-deficit-hyperactivity-disorder/
Bayard, F., Nymberg Thunell, C., Abé, C., Almeida, R., Banaschewski, T., Barker, G., Bokde, A. L. W., Bromberg, U., Büchel, C., Quinlan, E. B., Desrivières, S., Flor, H., Frouin, V., Garavan, H., Gowland, P., Heinz, A., Ittermann, B., Martinot, J.-L., Martinot, M.-L. P., & Nees, F. (2018). Distinct brain structure and behavior related to ADHD and conduct disorder traits. Molecular Psychiatry, 25(11), 10.1038/s41380-0180202-6. https://doi.org/10.1038/s41380-018-0202-6
Boston Children’s Hospital. (2024). Childrenshospital.org. https://www.childrenshospital.org/conditions/adhd
Miller, C. (2023, January 26). What Are Nonstimulant Medications for ADHD? Child Mind Institute; Child Mind Institute. https://childmind.org/article/what-are-nonstimulant-medications-for-adhd/
Radiological Society of North America. (2023, January 23). MRI Scans of Children's Brains [Photograph]. SciTech Daily. https://scitechdaily.com/brain-markers-of-adhd-identified-in-childrens-mri-scans/
Rodden, J. (2019, June 27). Non-Stimulant ADHD Medication Overview. ADDitude. https://www.additudemag.com/non-stimulant-adhd-medication/
Villines, Z. (2023, November 30). Frontal lobe: Functions, structure, and damage. Medical News Today. https://www.medicalnewstoday.com/articles/318139
Comments